Case Study: 43-Year-Old Male with Acute Ankle Pain
Clinical Presentation
A 43-year-old male presented with acute onset of ankle pain after stepping off a curb while walking from his office to the parking lot. He reported difficulty bearing weight and noticeable weakness during plantar flexion. No prior history of ankle injuries was noted.
History
Presentation: Sudden sharp pain in the posterior ankle region, followed by a "snapping" sensation.
Occupation: Office worker - accountant
Past Medical History: No significant history of musculoskeletal injuries.
Medications: None.
Lifestyle: Regular physical activity including recreational basketball.
Physical Examination
Swelling and tenderness localized to the posterior ankle.
A palpable gap was noted approximately 2–4 cm above the calcaneal insertion.
Weakness in plantar flexion and a positive Thompson test.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Diagnostic Steps
Ultrasound Findings:
The distal Achilles tendon (AT) shows mild hypoechogenicity due to anisotropy; however, its normal fibrillar pattern is intact, and it maintains a normal insertion onto the calcaneus (arrow in Fig. 7).
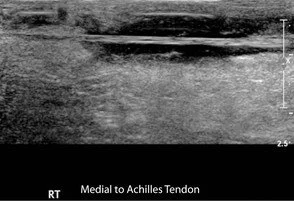
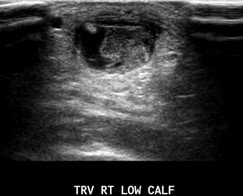
Sagittal views (Figs. 8 and 9) and a panoramic view (Fig. 10) of the upper AT reveal a full-thickness tear located approximately 2–4 cm proximal to the calcaneal insertion. The gap between the torn edges (arrows) is filled with heterogeneous material and fluid, also noted on transverse view (Fig. 11). The smaller plantaris tendon remains intact on the medial side (arrow in Fig. 12).
Fig. 7
Fig. 8
Fig. 9
Fig. 10
Fig. 11
Fig. 12
Differential Diagnosis
Partial Achilles tendon tear.
Tendinosis.
Final Diagnosis - Complete Rupture of Achilles Tendon
Key Teaching Points
Achilles tendon ruptures commonly occur in middle-aged men and are often associated with high-impact activities like basketball or sudden weight-bearing movements, such as stepping off a curb.
The injury typically involves a hypovascular area of the tendon, 2–4 cm above the calcaneal insertion. Ultrasound is a valuable diagnostic tool in identifying full-thickness tears, as it provides detailed visualization of tendon fiber disruption, retraction, and associated changes, such as fluid and fat herniation into the tendon gap.
US findings of complete AT tear:
Complete disruption of tendon fibers
Retraction of tendon, either tapered or balled up
Refractive shadowing at torn edge; can use to localize edge of torn tendon so as to accurately measure length of tendon gap
Gap may fill in with fluid, hemorrhage, or adjacent echogenic fat
Panoramic sagittal view of a second patient shows a full-thickness AT tear with retraction of the proximal tendon stump and herniation of echogenic fat (solid white arrow in Fig. 13) into the gap between the torn ends of the AT (red arrows). Linear refractive shadowing (dashed white arrow) indicates the torn edge of the distal tendon. Normal attachment of the distal AT to the calcaneus is seen (angled arrow).
Fig. 13
Dynamic imaging with US will reveal independent movement of the tendon stumps and increased retraction in cases of full-thickness tears.
Document the distance from the calcaneal insertion and myotendinous junction, as well as the length of the tendon gap in neutral position, flexion, and extension.
Pitfall: Confusing the medial plantaris tendon (Fig. 12) with residual intact AT fibers, which can mimic a partial tear.
The plantaris tendon may remain intact even in complete AT rupture.
Trace the plantaris tendon along its normal course between the gastrocnemius and soleus muscles.
Partial tear: Characterized by a hypoechoic or anechoic area/cleft partially disrupting the tendon fibers and fibrillar echopattern; may appear well-defined and associated with tendinosis.
Tendinosis: Presents as focal or diffuse fusiform tendon swelling, hypoechoic with intact fibers. Increased flow on power Doppler represents neovascularity (not inflammation) and correlates with symptoms
Management
Immobilization
Surgical repair
Reference
Scoutt LM, Hamper UM, Angtuaco TL, Scoutt LM, Hamper UM, Angtuaco TL, eds. Case 144. In: Ultrasound. Oxford University Press; 2016:0. doi:10.1093/med/9780199988105.003.0144